SANTA FE, New Mexico – The New Mexico Health Care Authority and the New Mexico Psychology Internship Consortia announce full accreditation from the American Psychology Association for their psychology internship program, dedicated to training, recruiting, and retaining behavioral health…
Behavioral Health Program
Supporting systems that help people and communities thrive since 1955

WICHE’s Behavioral Health Program (BHP) has two main goals:
- To help Western states best serve the behavioral health care needs of their residents
- To develop, prepare, and continuously improve the behavioral health care workforce
The WICHE BHP pursues these goals through diverse means in three priority areas:
- Systems improvement to contract directly with states to optimize their delivery of behavioral health care
- Workforce development to help states assess, plan for, and meet their behavioral health workforce needs with a focus on adoption of evidence-based practices
- Research, data, and evaluation to advance behavioral health knowledge and promote sound public policy
The BHP staff and consultants include psychologists, social workers, policy experts, researchers, and more – all who have earned strong reputations as thought leaders in their areas of expertise, and who are as passionate in their purpose as they are diverse in their skill sets.
Like other WICHE programs, the BHP expands the capabilities of its partners by promoting innovation, cooperation, resource-sharing, and sound public policy.
The BHP imagines a future in which no one, however emotionally or geographically isolated, is limited by behavioral health challenges.

Rural New Mexico Behavioral Health Internship Program Receives National Accreditation
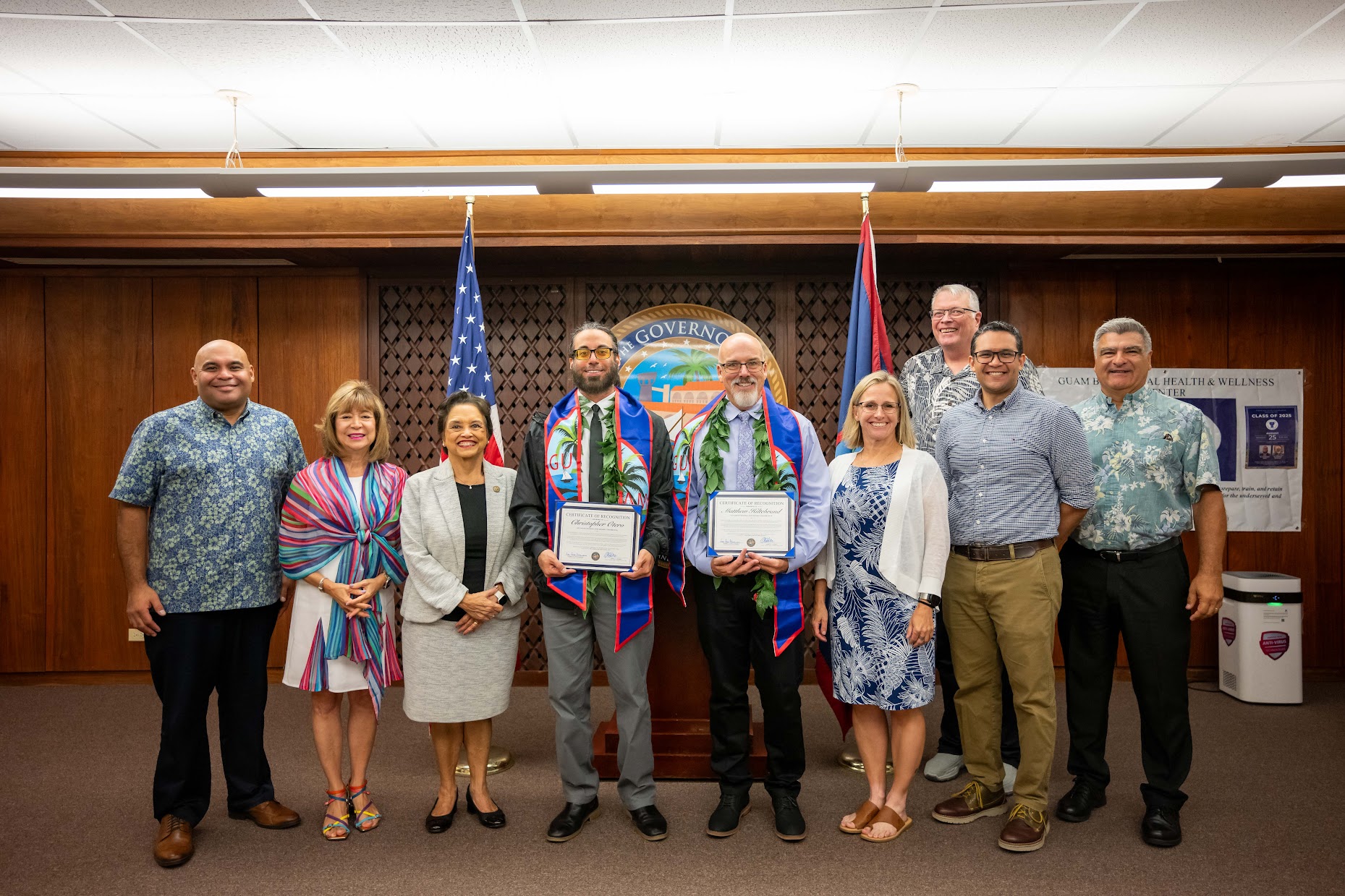
Guam is a 'go-to' destination for psychology interns
Guam is becoming an attractive training ground for doctoral psychology students thanks to the Guam Psychology Internship Consortium (GPIC), which, through partnership with the Guam Behavioral Health and Wellness Center (GBWHC) and the Western Interstate Commission for Higher Education (WICHE), has graduated the first two students to complete the recently accredited American Psychological Association (APA) doctoral program.



We support the administration of year-long programs for doctoral interns to build the behavioral health workforce pipeline, particularly in rural or remote areas, in six Western states.
We partner on a federally funded center to provide training, webinars on evidence-based practices, and providing Community of Practice learning opportunities. We aim to reach populations impacted by health disparities in rural, tribal, and frontier communities to reduce morbidity and mortality associated with opioid and/or stimulant use in rural communities.
In partnership with the U.S. Department of Veterans Affairs, we are developing and piloting a multi-platform suicide prevention program to assist veterans in rural communities.
- Rural Psychology Internship Consortia
- Mountain Plains Rural Opioid Technical Assistance Center (Mountain Plains ROTAC)
- Together with Veterans

WSDSG Meets In-person in Boulder, CO
The Western States Decision Support Group (WSDSG) held its annual in-person meeting in Boulder, CO on Nov. 18-19, 2024. The meeting included a reception and day-long conference that featured presentations from Dr. Michelle Cornette from the Substance Abuse and Mental Health Services Administration (SAMHSA) on 988 Lifeline and Crisis Services Program Evaluation, Kristin Neylon from the NASMHPD Research Institute (NRI) on National Trends in Behavioral Health Crisis Services, and Melanie Boetel and Brittney Lengkeek from the South Dakota Department of Social Services, Division of Behavioral Health on Using State Data to Track Outcomes and Inform Policy and Practice. The event provided opportunities for networking, information exchange, and planning, which included the formation of a WSDSG Steering Committee with representatives from Alaska, Nevada, South Dakota, Utah, and Washington.
Behavioral Health Publications